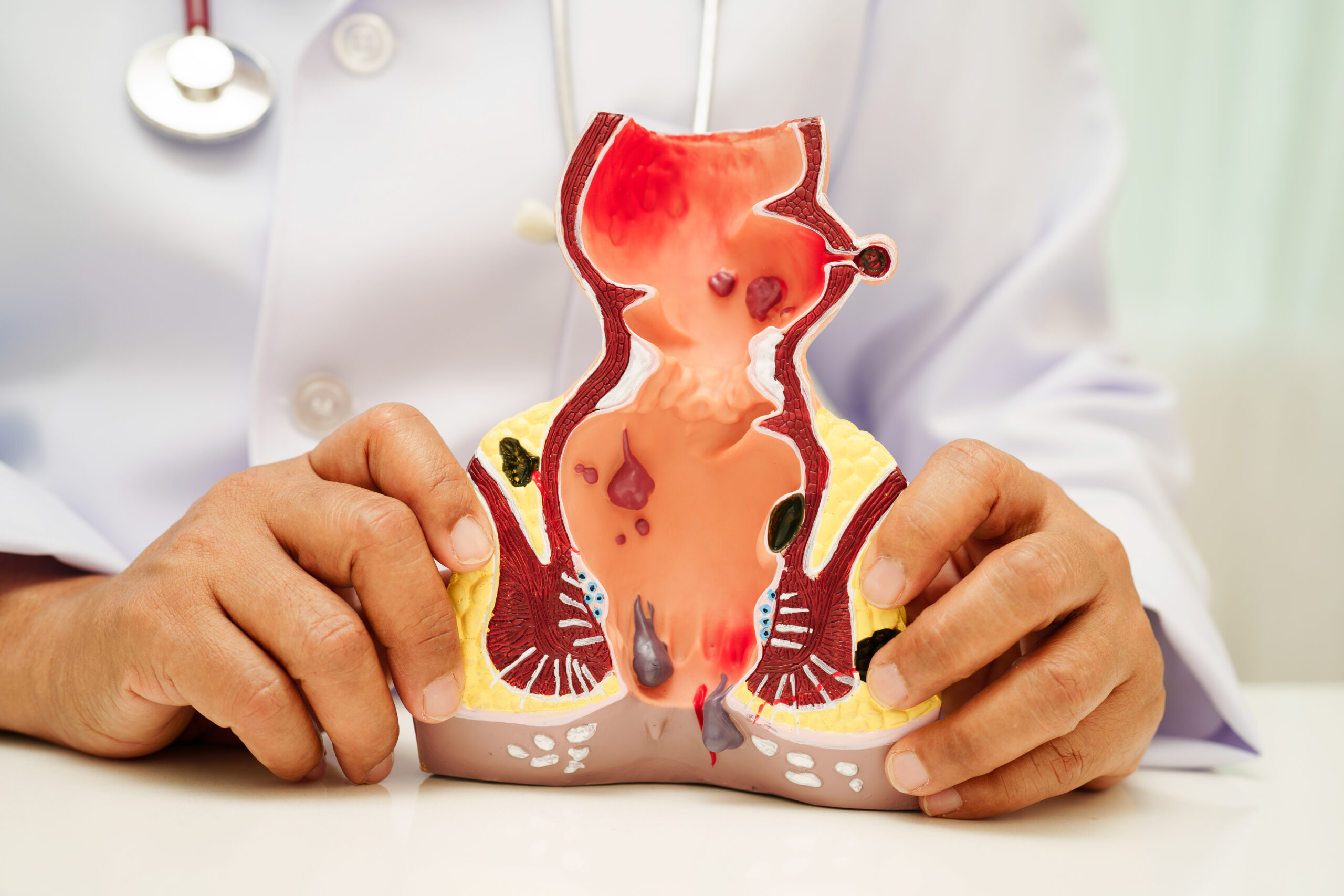
Fistula-in-ano is a difficult chronic condition that affect thousands of patients worldwide. A fistula is an abnormal connection between two body parts, often caused by an infection that creates a tunnel from an internal organ, like the anus, to the skin surface. In conventional treatment fistula usually requires surgery, drainage, or long-term care strategies. A common treatment many patients receive is repeated use of antibiotics. Frequent and prolonged use of antibiotics can delay healing, worsen symptoms, and lead to additional complications. The holistic, individualized approach of Ccube homoeopathy, under the guidance of Dr Rashmi Chandwani can support the body’s natural healing processes.
Understanding Fistula and Infection
A fistula usually starts with an infection of a gland or tissue. For instance, in anal fistulae, an initial abscess forms when bacteria invade and cause infection. This abscess might be surgically drained, but the resulting tunnel, known as a fistula tract, persists if underlying issues remain.
Since infections often lead to fistulae, antibiotics are frequently prescribed. However, antibiotics alone cannot close a fistula tract or resolve the ongoing inflammation. They may temporarily suppress bacteria but do not heal the fistula itself.
Antibiotics: Why They’re Used and What They Do
Antibiotics are medications that kill or prevent bacteria from growing. They can be lifesaving in acute infections. For a fistula with an active infection or abscess, antibiotics help control bacterial growth and manage systemic symptoms like fever or cellulitis. However, in these cases, antibiotics are usually supportive rather than curative. Their blind and repeated use has significant downsides when used long-term or without clear reasons.
How Repeated Antibiotics Can Delay Healing ?
Let’s look at how repeated antibiotic use can hinder healing in fistula patients:
-
Imbalance in Normal Microbiota
Our bodies contain a complex community of microbes that play important roles in immune regulation, digestion, and tissue health. Repeated antibiotic use disrupts these normal bacterial populations in the gut, skin, and mucosa, leading to an imbalance known as dysbiosis. Healthy microbiota help control harmful bacteria and support immune function. When this balance is disturbed:
- Barrier functions weaken.
- Immune responses become unregulated.
- Opportunistic pathogens may thrive.
- Tissue repair processes can suffer.
For a fistula patient, instead of restoring balance, repeated antibiotics can make tissues more prone to ongoing inflammation.
-
Antibiotic Resistance
A major concern in modern medicine is antibiotic resistance. With frequent antibiotic use, bacteria can adapt and survive future treatments. This means:
- Infections become harder to treat.
- Stronger bacteria may develop.
- Patients may find themselves in a cycle of escalating medications with diminishing effectiveness.
Antibiotic resistance can lengthen recovery time, increase symptoms, and require stronger, more harmful drugs, none of which address the underlying issue.
-
Suppression of Beneficial Immune Signals
The immune system depends on precise signals to manage inflammation and healing. Antibiotics blunt bacterial signals that sometimes trigger appropriate immune responses. This can delay the immune system’s ability to:
- Recognize and eliminate lingering pathogens.
- Clear damaged cells.
- Begin repair mechanisms.
Because healing relies on a balanced immune response, its disruption may unintentionally prolong inflammation and tissue damage.
-
Masking Symptoms but Not Healing
Antibiotics can sometimes hide symptoms like fever, swelling, or discharge without fully removing the underlying cause. This creates a false sense of improvement. The fistula tract continues to be inflamed, and symptoms return once antibiotics stop, leading to repeated treatments. This cycle delays actual recovery and encourages reliance on drugs instead of addressing root problems.
-
Potential Side Effects and Complications
Aside from microbial imbalance and resistance, repeated antibiotic use can cause:
- Gastrointestinal upset.
- Yeast infections.
- Allergic reactions.
- Stress on organs like the liver and kidney.
These side effects further weaken the patient, making healing even slower.
Can antibiotics delay wound healing?
Yes, repeated or unnecessary use of antibiotics can sometimes delay wound healing. In fact:
- Overuse can disturb the natural bacterial balance (gut microbiome).
- It may weaken immunity over time.
- It can lead to antibiotic resistance.
- It may reduce collagen formation, which is essential for wound repair.
- It can mask symptoms without treating the root cause.
In chronic wounds like fistula or recurrent abscess, antibiotics often give temporary relief but do not eliminate the underlying tract or internal infection source. Proper drainage, immunity support, nutrition, and treating the root cause are essential for complete healing.
What can slow down fistula healing?
Fistula healing can be slow due to multiple factors:
- Persistent internal infection or undrained abscess
- Poor digestion and chronic constipation
- Diabetes or uncontrolled blood sugar
- Repeated antibiotic usage
- Poor hygiene around the anal region
- Weak immunity
- Smoking
- Inadequate protein intake
- Stress and lack of sleep
A fistula is not just a surface wound; it is an abnormal tunnel between the anal canal and skin. Unless the internal opening is addressed and the body’s healing capacity is strengthened, recurrence is common.
Why is my fistula wound not healing?
If your fistula wound is not healing, possible reasons include:
- The internal tract is still active.
- Continuous infection inside the tunnel.
- Improper wound care.
- Excess moisture or friction in the area.
- Recurrent abscess formation.
- Poor nutritional status.
- Low immunity.
- Chronic inflammatory conditions (like Crohn’s disease).
In many cases, people focus only on the external wound. However, fistula healing requires addressing the internal communication, reducing infection, and improving overall immunity.
A Better Way? The Role of Ccube homoeopathy
At Ccube homoeopathy, under the care of Dr Rashmi Chandwani, we understand that true healing of a fistula requires more than just fighting infections with drugs. Healing involves restoring the body’s internal balance, reducing chronic inflammation, and supporting immune health.
Ccube homoeopathy – Pioneer in Holistic Fistula Care
Ccube homoeopathy has become a leader in holistic management of chronic conditions like fistula. Under Dr Rashmi Chandwani’s guidance, Ccube homoeopathy combines classical homeopathic methods with an individualized understanding of each patient, focusing on solving root causes instead of just masking symptoms. At Ccube homoeopathy, we evaluate each patient not only for physical symptoms but also for their unique emotional, mental, and constitutional profile.
This comprehensive assessment allows Dr Rashmi Chandwani to prescribe remedies that resonate with the patient’s overall health pattern, rather than targeting only localized inflammation. This method supports the body’s healing pathways and encourages immune function and tissue repair without the negative effects of repeated antibiotic use. Moreover, Ccube homoeopathy acknowledges that chronic fistulae often involve deeper systemic issues. By using personalized remedies, providing lifestyle guidance, offering dietary recommendations, and allowing time, healing can become a sustainable process.
Many patients who faced frustrating cycles of antibiotics, recurrent pain, and delayed recoveries have found relief through the careful care at Ccube homoeopathy. Treatments focus on understanding patients and guiding them toward lasting balance, resilience, and well-being.
Final Thoughts
Repeated antibiotic use may seem like an easy fix for recurring fistula infections, but it can unintentionally delay healing by disrupting the microbiome, promoting resistance, masking symptoms, and upsetting immune balance. True resolution comes not from endless cycles of medication but from restoring the body’s natural ability to heal. Ccube homoeopathy, under the expertise of Dr Rashmi Chandwani, offers a compassionate, personalized path to healing that addresses the whole body. By recognizing each patient’s unique constitution and supporting the systems that drive recovery, Ccube homoeopathy leads the way in fistula care, promoting lasting health rather than temporary fixes.
If you or someone you know has faced ongoing fistula symptoms and repeated antibiotic treatments, consider looking into holistic, root-focused care. Healing is not simply about suppressing symptoms, it’s about restoring balance. At Ccube homoeopathy, that journey starts with understanding, empathy, and science-informed homeopathic care.
FAQs
1. Can antibiotics cure a fistula permanently?
No. Antibiotics can control active infection or reduce symptoms temporarily, but they cannot close or heal the fistula tract. A fistula is an abnormal tunnel, and unless the root cause and internal opening are addressed, it often keeps recurring.
2. Can repeated antibiotics make a fistula worse?
Repeated or long-term antibiotic use can delay healing by disturbing the gut microbiome, weakening immune response, and promoting antibiotic resistance. It may also mask symptoms without resolving the underlying problem, leading to repeated flare-ups.
3. Why is my fistula wound not healing even after treatment?
Common reasons include an active internal tract, ongoing infection, poor immunity, improper wound care, chronic constipation, diabetes, poor nutrition, or repeated abscess formation. Healing requires treating the internal cause, not just the external wound.
4. What factors slow down fistula healing?
Fistula healing can be slowed by persistent infection, weak immunity, repeated antibiotic use, poor hygiene, smoking, stress, lack of sleep, poor nutrition (especially low protein), and conditions like diabetes or Crohn’s disease.
5. How can a holistic approach like Ccube homoeopathy help in fistula?
A holistic approach focuses on strengthening immunity, reducing chronic inflammation, and addressing the root cause rather than just suppressing symptoms. At Ccube homoeopathy, treatment is individualized under Dr Rashmi Chandwani’s guidance to support the body’s natural healing process and promote long-term recovery.